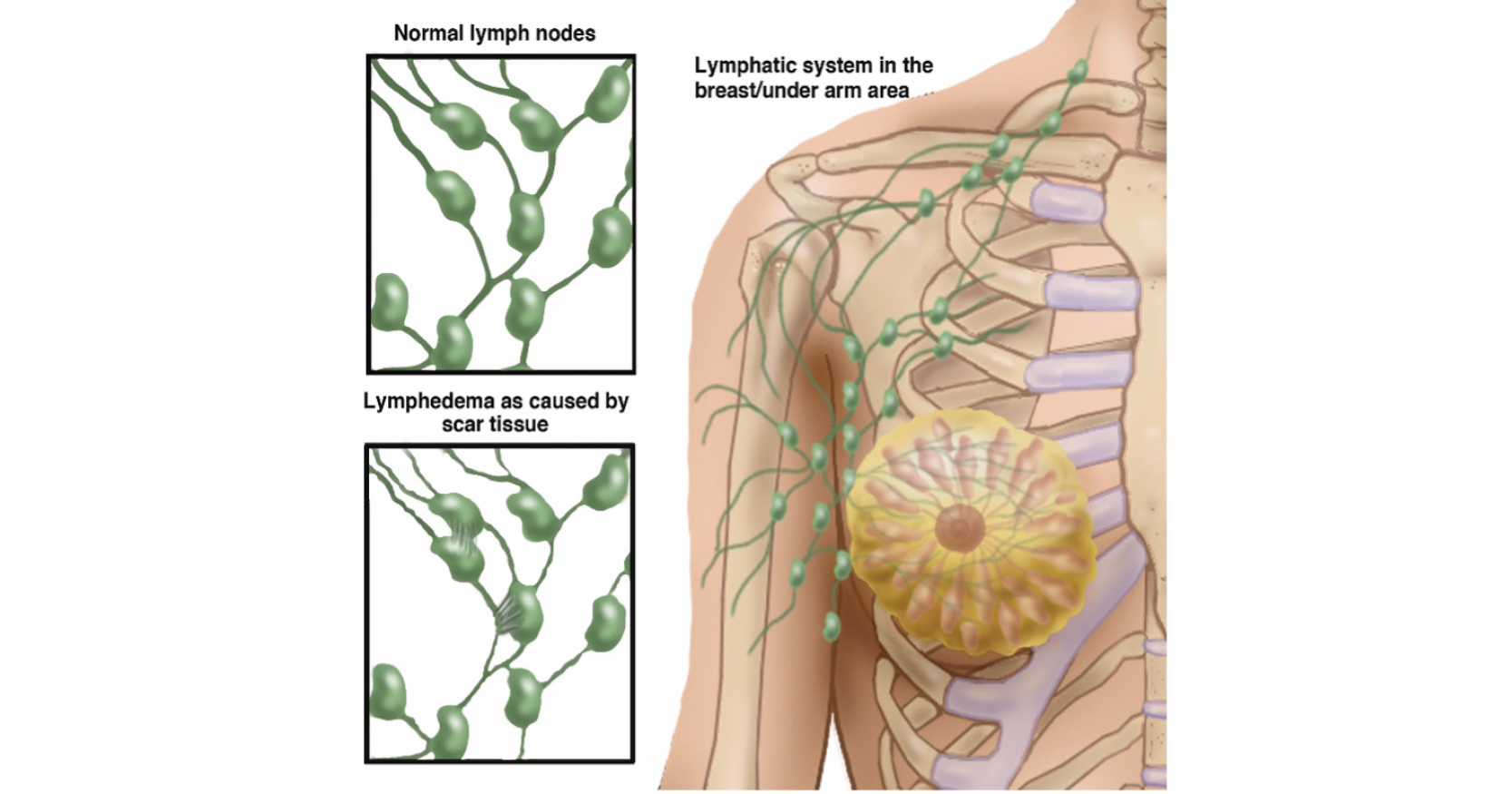
<p>This case study highlights the challenges faced by patients with lymphatic filariasis and the success of an integrated home-based self-care programme developed at the Institute Of Applied Dermatology in Kerala, South India. This innovative treatment regimen uses integrated practice to fuse modern dermatology techniques with traditional Indian methods such as yoga and Ayurvedic medicine.</p>